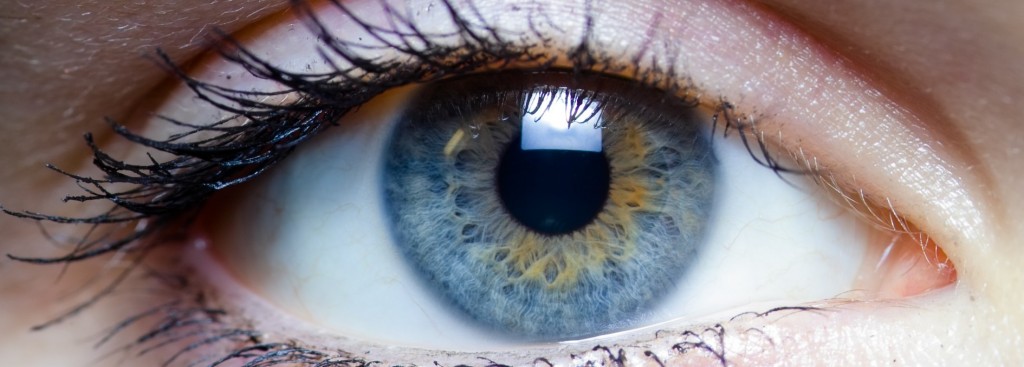
Cornea
The cornea is a thin, clear, spherical layer of tissue on the surface of the eye that provides a window for light to pass through. In a healthy eye, the cornea bends or refracts light rays so they focus precisely on the retina in the back of the eye.
There are many diseases that can affect the cornea, causing pain or loss of vision. Disease, infection or injury can cause the cornea to swell (called "edema") or degrade (become cloudy and reduce vision). Common diseases and disorders that affect the cornea include:
- Allergies
- Conjunctivitis ("Pink Eye")
- Dry Eye
- Corneal Dystrophies including Fuchs' Dystrophy and
Lattice Dystrophy - Glaucoma (High Eye Pressure)
- Infections
- Keratitis (Viral Inflammation)
- Keratoconus
- Ocular Herpes
- Pterygium
- Shingles (Herpes Zoster)
- Stevens-Johnson Syndrome
Treatment for corneal disease can take many forms, depending on the underlying problem as well as the patient's preferences. Some conditions resolve on their own and many can be treated with medication. If the cornea is severely damaged or if there is a risk of blindness, a corneal transplant may be recommended to preserve vision.
Fuchs’ Dystrophy
Fuchs’ dystrophy is an inherited eye disease that causes the cells in the endothelium, the last layer of the cornea, to deteriorate. This leads to distorted vision and corneal swelling. The exact cause of Fuchs’ dystrophy is unknown, but is believed to be a combination of hereditary, hormonal and inflammatory factors. This condition affects both eyes and is more common in women than in men.
The cornea is made up of five different layers, each of which has a specific function that controls vision. The endothelium is the back layer of the cornea, which removes excess fluid from the cornea. Excess fluid can cause the cornea to swell and vision to become distorted. Occasionally the swelling can become so severe that bullae (blister like lesions) will develop that can result in pain. Once endothelial cells are lost, they do not grow back, so this condition will continue to progress with time.
Symptoms of Fuch's Dystrophy
Although this condition is inherited, symptoms do not usually appear until the patient is over the age of 50. Patients with Fuchs’ dystrophy may experience blurred vision as the first sign of this condition. Blurred vision occurs as a result of fluid accumulating in the cornea while you sleep. As this fluid evaporates throughout the day, vision will improve. Other symptoms of Fuchs’ dystrophy may include:
- Sensitivity to bright lights
- Halos around lights
- Poor night vision
- Sharp pains in the eyes
- Sandy, gritty sensation in the eyes
- Fluctuating vision
DSAEK (Partial Cornel Transplants)
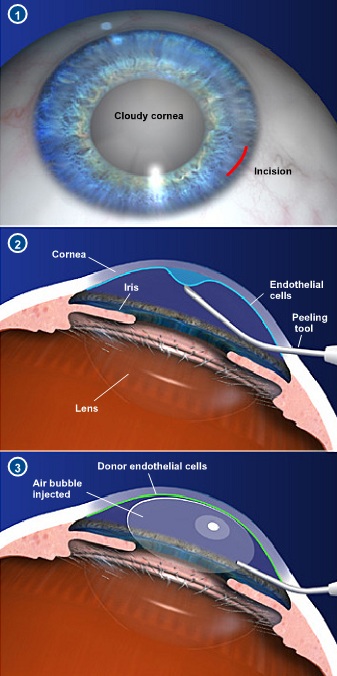 Corneal transplants have restored vision to thousands of patients who have suffered vision loss from corneal disease, infection or injury. Recently an innovative new technique: Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) has allowed for transplantation of the rear or endothelial only layer of the cornea. The advantage of DSAEK over a full corneal transplant is that there is little change in the shape of the cornea and therefore less change in the patient’s prescription. This means that the patient is less likely to need special contact lenses to see properly after surgery. There are also less sutures which results in more comfort during healing and a lower likelihood of infection. Vision recovery is also much quicker and organ rejection is less likely to occur. The bottom line is that DSAEK is the preferred method to correct vision loss from certain eye disease because it is safer, success rates are higher and vision recovery is quicker.
Corneal transplants have restored vision to thousands of patients who have suffered vision loss from corneal disease, infection or injury. Recently an innovative new technique: Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) has allowed for transplantation of the rear or endothelial only layer of the cornea. The advantage of DSAEK over a full corneal transplant is that there is little change in the shape of the cornea and therefore less change in the patient’s prescription. This means that the patient is less likely to need special contact lenses to see properly after surgery. There are also less sutures which results in more comfort during healing and a lower likelihood of infection. Vision recovery is also much quicker and organ rejection is less likely to occur. The bottom line is that DSAEK is the preferred method to correct vision loss from certain eye disease because it is safer, success rates are higher and vision recovery is quicker.
To perform DSAEK, the surgeon cuts and prepares the donor cornea. Next, he or she makes a mark in the surface of the patient's cornea with a trephine (an instrument used to cut circular sections of tissue). That mark serves two purposes: it helps the surgeon determine what size the transplant should be, and it outlines the area of the patient's cornea that needs to be peeled away.
Next, the surgeon scores the damaged section of the cornea and strips the membrane away from the eye. Then the donor cornea is folded into a "taco" shape and placed in the eye. A single stitch closes the incision. Patients are sent to the recovery room for about one hour then allowed to return home. Patients are then given antibiotics and steroid eye drops and will return the next day for a follow-up appointment.
Keratoconus
Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to bulge into a cone-like shape. The cornea is the clear, central part of the surface of the eye. As the cornea becomes more irregular in shape, it causes progressive nearsightedness and astigmatism resulting in distorted and blurred vision. Glare and light sensitivity also may be noticed. Keratoconic patients often have frequent prescription changes.
Symptoms of Keratoconus
Keratoconus often begins to develop in the teen years to the early 20s, although it can develop at any age. Changes in the shape of the cornea occur gradually, usually over several years. In most patients with keratoconus, both eyes eventually become affected.
Keratoconus can be difficult to detect because it usually develops very slowly. Signs of keratoconus may include:
- Distorted and blurred vision
- Myopia (nearsightedness)
- Astigmatism
- Double vision
- Headaches due to eye strain
- Glare
- Light sensitivity
Keratoconus Treatment Options
In the early stages of keratoconus, glasses or soft contact lenses may help to correct the nearsightedness and astigmatism associated with the disease. As the condition progresses and the cornea becomes increasingly thin, more advanced treatment is required.
Rigid Gas-Permeable Contact Lenses – If eyeglasses or regular soft contact lenses cannot control keratoconus, rigid gas-permeable (RGP) contact lenses are usually the preferred treatment. The rigid lens covers the cornea, replacing the cornea's irregular shape with a smooth, uniform refracting surface, improving vision.Rigid contact lenses can be less comfortable to wear than soft lenses. Further, fitting contact lenses on a cornea with keratoconus can be challenging and time-consuming. If you are using RGP contact lenses, you will need to visit your doctor frequently to fine-tune the fit and prescription of the lenses, especially if your keratoconus continues to progress.
INTACS 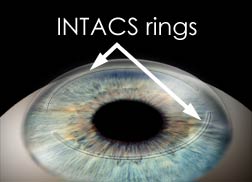 INTACS are plastic rings inserted into the mid-layer of the cornea to flatten it, changing the shape and location of the cone. INTACS may be needed when the distorted vision from keratoconus can no longer be corrected with contact lenses or eyeglasses. Intacs inserts remodel and reinforce your cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide you with improved vision. The implants are removable and exchangeable. The placement of Follow-up visits will be required to monitor the healing process and evaluate the visual benefits of the procedure. Even after a successful procedure, glasses or contacts still may be required to provide you with good vision. Dr. Dean Dornic is one of the most experienced Intacs surgeons in the mid-Atlantic region. To find out if you are a candidate for Intacs arrange a surgical consultation. For more information on Intacs for the treatment of keratoconus, visit www.intacsforkeratoconus.com
INTACS are plastic rings inserted into the mid-layer of the cornea to flatten it, changing the shape and location of the cone. INTACS may be needed when the distorted vision from keratoconus can no longer be corrected with contact lenses or eyeglasses. Intacs inserts remodel and reinforce your cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide you with improved vision. The implants are removable and exchangeable. The placement of Follow-up visits will be required to monitor the healing process and evaluate the visual benefits of the procedure. Even after a successful procedure, glasses or contacts still may be required to provide you with good vision. Dr. Dean Dornic is one of the most experienced Intacs surgeons in the mid-Atlantic region. To find out if you are a candidate for Intacs arrange a surgical consultation. For more information on Intacs for the treatment of keratoconus, visit www.intacsforkeratoconus.com
Collagen cross-linking is a relatively new method for treating keratoconus. It works by strengthening the corneal tissue to stop it from bulging. In this procedure, eye drops containing riboflavin (vitamin B2) are applied to the cornea and then activated by ultraviolet light. This strengthens the collagen fibers within the cornea. Corneal collagen cross-linking can reverse some of the corneal steepening and astigmatism caused by keratoconus. Numerous studies have validated the value of corneal collagen cross-linking in keratoconus. In some cases, corneal collagen cross-linking can postpone or negate the need for a corneal transplant.
Corneal Transplant Surgery is needed for patients with advanced keratoconus, where other therapies no longer provide clear vision. This usually occurs in 15-20% of cases. In corneal transplant surgery, most of the cornea is removed and then replaced with a new donor cornea. The results of the procedure have a success rate of over 97%.